The Assisted Dying Bill is one of modern British history’s most contentious legal proposals. Designed to give terminally ill individuals the right to end their lives with medical assistance, it has reignited passionate debates across the spectrum of law, ethics, and society. Supporters hail it as a compassionate and progressive step towards respecting autonomy and alleviating suffering, while critics warn of the profound risks it could introduce.
This blog delves into the Assisted Dying Bill’s provisions, the arguments for and against it, international precedents, and its broader implications for legal and ethical frameworks.
Understanding the Assisted Dying Bill
At its core, the Assisted Dying Bill aims to legalize the practice of assisted dying for terminally ill adults in England and Wales. It focuses on granting individuals the autonomy to choose their end-of-life journey. Under the current draft:
- Only adults diagnosed with a terminal illness, with a prognosis of six months or less to live, can apply.
- Two independent doctors must verify that the individual meets the medical and psychological requirements, ensuring the decision is well-informed, voluntary, and devoid of external pressure.
- Final approval lies with a High Court judge, who reviews the case to confirm adherence to legal safeguards.
- The process mandates that individuals self-administer the life-ending medication, further ensuring voluntariness.
This careful construction reflects an effort to mitigate concerns about potential abuse, while addressing the growing demand for greater control over life’s final chapter.
Why the Bill Is So Controversial
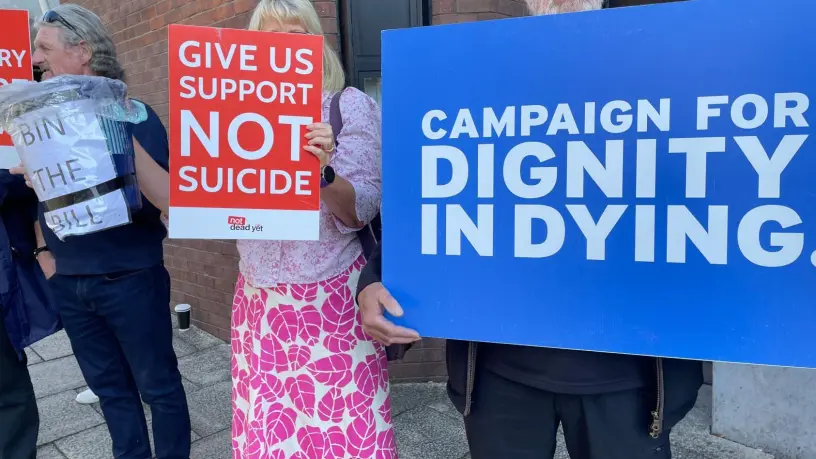
The debate surrounding the Assisted Dying Bill is deeply polarizing because it addresses fundamental questions about life, death, and the role of law and medicine in governing them. While proponents advocate for compassion and autonomy, opponents express fears about potential risks, moral boundaries, and unintended consequences.
Support for the Assisted Dying Bill
The driving force behind the bill is the need to provide terminally ill individuals with a dignified and pain-free way to end their lives. Advocates highlight several key benefits:
- Respect for Autonomy: At its heart, the bill empowers individuals to make decisions about their own lives. For terminally ill patients facing inevitable death, choosing how and when to die can be a profound assertion of personal freedom.
- Alleviating Suffering: Terminal illnesses often bring prolonged and unbearable physical and emotional suffering. Proponents argue that modern medicine, while adept at prolonging life, often fails to address the quality of that extended life. Assisted dying offers a humane alternative to unnecessary suffering.
- Global Trends and Public Opinion: Countries like Canada, Belgium, and parts of the United States have embraced assisted dying with carefully designed safeguards. Surveys in the UK consistently reveal strong public support for the principle of assisted dying, particularly among younger and middle-aged demographics.
Criticism of the Assisted Dying Bill
Opponents of the bill raise concerns that extend beyond individual cases, warning of societal, ethical, and practical risks:
- The Slippery Slope Argument: One of the most common fears is that legalizing assisted dying could lead to its gradual expansion. Critics point to countries like Belgium and the Netherlands, where initial laws restricted assisted dying to terminally ill adults but have since expanded to include individuals with psychiatric conditions and, in rare cases, minors.
- Coercion and Vulnerability: There is a real risk that vulnerable individuals, such as the elderly or disabled, may feel pressured to choose assisted dying to relieve perceived burdens on their families or society. Despite safeguards, detecting subtle coercion can be challenging.
- The Role of Medical Professionals: Assisted dying fundamentally alters the role of healthcare providers, asking them to participate in actions traditionally seen as contrary to their Hippocratic Oath. Many doctors feel that their responsibility is to preserve life, not end it.
- Impact on Palliative Care: Critics worry that legalizing assisted dying might divert attention and resources from improving palliative care. The focus, they argue, should be on providing holistic and compassionate end-of-life care rather than facilitating death.
International Precedents: Lessons from Belgium and Canada
The UK is not the first country to grapple with the complexities of assisted dying. Belgium, where euthanasia has been legal since 2002, and Canada, which introduced Medical Assistance in Dying (MAID) in 2016, offer valuable insights.
In Belgium, the law initially applied to terminally ill adults but has since expanded under strict conditions to include children and individuals with severe mental illnesses. This expansion has sparked controversy, with critics warning of “mission creep.” However, supporters argue that it reflects a commitment to respecting individual autonomy.
Canada’s experience is more recent but similarly illuminating. The MAID program has been lauded for its rigorous safeguards and comprehensive support systems. Yet, it has also faced criticism, particularly for cases where individuals chose assisted dying due to inadequate access to healthcare or social services.
The UK Debate: A Shift in Perspectives
When the UK Parliament last debated assisted dying in 2015, the proposal was overwhelmingly rejected. However, public opinion and political attitudes have shifted significantly since then.
MPs are no longer voting strictly along party lines, reflecting the deeply personal nature of the issue. While the government has maintained a neutral stance, several high-profile ministers have expressed reservations. At the same time, grassroots campaigns and personal testimonies have brought new urgency to the debate.
Legal and Ethical Implications
Legalizing assisted dying would mark a profound shift in the UK’s legal and ethical landscape. It raises complex questions about the limits of personal freedom, the role of the state in protecting vulnerable citizens, and the evolving nature of medical ethics.
Balancing Rights and Responsibilities
One of the central legal challenges is balancing individual autonomy with the state’s responsibility to protect its most vulnerable citizens. The High Court’s involvement as a safeguard underscores the seriousness of these decisions and the need for rigorous oversight.
Redefining Medical Ethics
Legalizing assisted dying would fundamentally alter the relationship between patients and healthcare providers. It would require a rethinking of medical ethics, training, and support systems to ensure that practitioners can navigate these challenges compassionately and professionally.
Conclusion: A Defining Moment in British Law and Society
The Assisted Dying Bill is more than a piece of legislation—it is a reflection of profound societal changes and evolving attitudes toward life, death, and individual autonomy.
While it offers a compassionate solution for those facing unbearable suffering, it also poses significant challenges. Safeguards must be meticulously designed and implemented to prevent misuse and ensure that the law remains a force for good.
As the debate continues, it is clear that the Assisted Dying Bill has the potential to reshape not only end-of-life care but also the very fabric of how we approach human dignity and autonomy. Whatever the outcome, the conversation it has sparked is vital in advancing our understanding of one of life’s most difficult and inevitable transitions.
The Assisted Dying Bill is a proposed law in the UK that allows terminally ill adults with less than six months to live to seek medical assistance to end their lives. It includes strict safeguards, such as verification by two doctors and approval by a High Court judge, to ensure the process is voluntary and free from coercion.
Supporters of assisted dying argue it respects personal autonomy and alleviates suffering for terminally ill patients. Opponents, however, raise concerns about potential coercion, a slippery slope toward broader euthanasia practices, and the ethical challenges it poses for medical professionals.
Countries like Canada, Belgium, the Netherlands, and several U.S. states have legalized assisted dying under strict conditions. These laws often include safeguards to ensure voluntariness, medical approval, and judicial oversight.